Discover the fascinating world of cochlear implants! This technology offers individuals with severe hearing loss a chance to reconnect with sound, improve communication, and experience a fuller life. Our comprehensive guide delves into the anatomy of the ear, explains how cochlear implants work, and explores the key steps involved in candidacy, evaluation, surgery, and rehabilitation. We also discuss the ethical and social implications of this technology, share inspiring success stories, and provide a glimpse into the promising future of hearing restoration through advancements like AI and brain-computer interfaces. Whether you’re considering cochlear implants for yourself or loved ones, or simply curious about this groundbreaking technology, this guide offers valuable insights and resources.
Introduction to Cochlear Implants
Cochlear implants are small, electronic devices that provide a sense of sound to individuals with severe hearing loss or profound deafness. Unlike hearing aids, which amplify sound waves, cochlear implants bypass damaged parts of the inner ear and directly stimulate the auditory nerve. This creates a new pathway for sound information to reach the brain, potentially allowing recipients to understand speech and perceive sounds they otherwise could not.
Overview of Hearing Loss
Hearing loss is a widespread condition affecting people of all ages and backgrounds. It affects the ability to detect and understand sound, ranging from mild muffling to complete deafness.
Types of Hearing Loss:
- Conductive hearing loss: Sound waves are unable to reach the inner ear due to problems in the outer or middle ear, often caused by earwax buildup, middle ear infections, or eardrum perforations.
- Sensorineural hearing loss: Damage to the inner ear or auditory nerve prevents sound signals from being transmitted to the brain effectively, often caused by age, noise exposure, genetic factors, illness, or ototoxic medications.
- Mixed hearing loss: A combination of conductive and sensorineural hearing loss.
Causes of Hearing Loss:
- Age-related hearing loss (presbycusis): Most common cause, affecting nearly half of adults over 75.
- Noise-induced hearing loss: Long-term exposure to loud sounds, like music, construction, or firearms.
- Genetic factors: Some individuals are genetically predisposed to hearing loss.
- Illness or injury: Head trauma, infections like meningitis, or certain medications can damage the ear.
Impact of Hearing Loss:
- Difficulty understanding speech, especially in noisy environments.
- Social isolation and communication challenges.
- Decreased work performance and educational opportunities.
- Emotional and psychological effects like frustration, fatigue, and anxiety.
Evolution of Hearing Aids and Cochlear Implants
Hearing aids:
- History dates back centuries, initially with passive devices like ear trumpets.
- Modern hearing aids electronically amplify sound waves, helping with mild to moderate hearing loss.
- Advancements include digital technology, directional microphones, and Bluetooth connectivity.
Cochlear implants:
- Developed in the mid-20th century for individuals with severe hearing loss or deafness.
- Surgically implanted device bypasses damaged parts of the inner ear and directly stimulates the auditory nerve.
- Enables recipients to perceive a wider range of sounds and improve speech understanding.
- Ongoing advancements improve sound quality, reduce distortion, and increase user comfort.
Importance of Cochlear Implants in Hearing Restoration
While hearing aids are incredibly beneficial for many, they have limitations for those with severe hearing loss. Cochlear implants offer a unique solution in such cases:
- Restore access to a broader range of sounds: Cochlear implants directly stimulate the auditory nerve, providing access to higher-frequency sounds often lost in sensorineural hearing loss.
- Improve speech understanding: Cochlear implants can significantly improve the ability to understand speech, even in noisy environments, enhancing communication and social interaction.
- Positive impact on quality of life: Studies show improved quality of life, emotional well-being, and social participation in cochlear implant recipients.
However, it’s important to understand:
- Not a cure: Implants do not restore normal hearing and require ongoing rehabilitation.
- Not for everyone: Candidacy depends on type and severity of hearing loss, individual needs, and lifestyle factors.
- Investment of time and resources: Surgery, rehabilitation, and device costs require careful consideration.
Anatomy of the Ear and Hearing Mechanism
The ear plays a crucial role in our sense of hearing and balance. It can be divided into three main parts:
-
Outer Ear: This visible part collects sound waves and channels them through the ear canal to the eardrum.
-
Middle Ear: The eardrum vibrates with incoming sound waves and transmits these vibrations to three tiny bones called ossicles (malleus, incus, and stapes). These bones amplify the sound and pass it to the oval window of the inner ear.
-
Inner Ear: This complex structure houses the cochlea, which is responsible for converting sound vibrations into electrical signals. The cochlea is filled with fluid and lined with tiny hair cells. When sound waves reach the oval window, they create movement in the fluid, which bends the hair cells. This bending triggers the hair cells to send electrical signals along the auditory nerve to the brain, where they are interpreted as sound.
Structure and Function of the Inner Ear
The inner ear can be further divided into two main parts:
-
Cochlea: This snail-shaped structure is the main organ of hearing. It is filled with fluid and divided into three chambers by a thin membrane. Hair cells are located along the basilar membrane, which separates the upper and lower chambers. Different frequency sounds cause vibration in different regions of the basilar membrane, allowing the hair cells to detect and respond to specific frequencies.
-
Vestibular system: This system consists of semicircular canals and otolith organs, which are responsible for balance and spatial orientation. The semicircular canals detect head rotation, while the otolith organs sense gravity and linear acceleration.
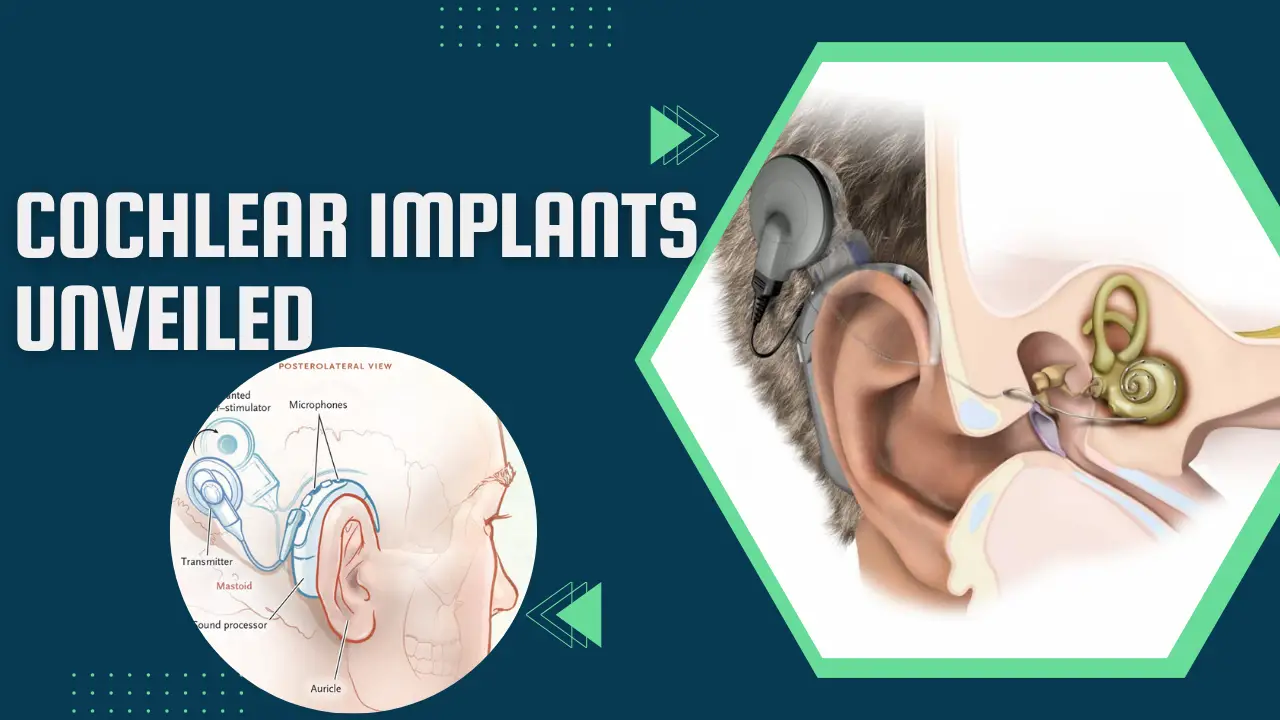
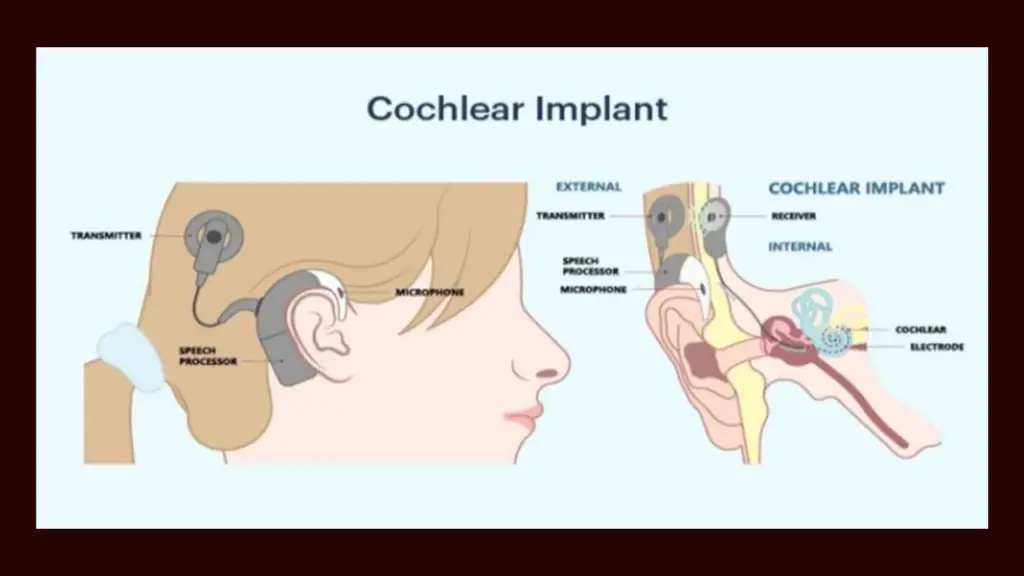
How Cochlear Implants Work
Cochlear implants are designed to bypass damaged hair cells in the inner ear and directly stimulate the auditory nerve. They consist of several components:
- External processor: This worn behind the ear captures sound waves and converts them into electrical signals.
- Receiver/stimulator: This surgically implanted device under the skin receives the electrical signals from the processor and converts them into electrical pulses.
- Electrode array: This thin electrode is inserted into the cochlea and stimulates the auditory nerve at various points, depending on the incoming sound frequency.
When someone with a cochlear implant hears a sound, the external processor captures the sound waves and transmits them to the receiver/stimulator. The receiver/stimulator converts the sound information into electrical pulses and sends them to the electrode array in the cochlea. The electrode array stimulates the auditory nerve, which then sends signals to the brain where they are interpreted as sound.
Neural Processing of Sound Signals
The auditory nerve carries the electrical signals from the cochlea to the brainstem, where they are processed by several auditory nuclei. These nuclei further refine the sound information, extracting features like pitch, loudness, and location. From the brainstem, the signals travel to the auditory cortex in the temporal lobe of the brain, where they are interpreted as meaningful sounds like speech, music, or environmental noises.
The neural processing of sound is a complex process that involves many different areas of the brain. This complex system allows us to not only hear sounds but also to understand their meaning and significance in our environment.
Candidacy and Evaluation for Cochlear Implants
Determining suitability for cochlear implants involves careful consideration of various factors through a comprehensive evaluation process. Here’s a breakdown:
Criteria for Cochlear Implant Candidacy:
- Type and severity of hearing loss: Individuals with severe to profound sensorineural hearing loss typically qualify. Conductive hearing loss is usually addressed with hearing aids instead.
- Age: Cochlear implants can benefit both adults and children (usually over 12 months), with specific eligibility criteria for each age group.
- Overall health: Good general health and ability to undergo surgery are crucial.
- Motivation and realistic expectations: Strong motivation and realistic understanding of the benefits and limitations of the implant are essential.
- Support system: Having a supportive network for rehabilitation and ongoing adjustment is important.
Pre-Implantation Evaluation Process:
The evaluation process is comprehensive and involves various specialists:
- Otolaryngologist (ENT): Examines the ears to ensure suitability for surgery and rules out any medical conditions that could pose risks.
- Audiologist: Conducts detailed hearing tests to assess the type and severity of hearing loss, speech understanding, and candidacy for different implant types.
- Speech-language pathologist: Evaluates communication skills and ability to participate in rehabilitation after implantation.
- Psychologist: Assesses motivation, expectations, and emotional readiness for the implant and its implications.
Medical and Audiological Assessments:
Several assessments are vital during the evaluation process:
- Medical history and physical examination: To identify any health conditions that could impact surgery or implant safety.
- Audiometric assessment: Measures hearing thresholds at different frequencies using pure tones and speech tests.
- Tympanometry: Assesses middle ear function.
- Vestibular evaluation: Evaluates balance function.
- Imaging studies: CT scans or MRIs to visualize the inner ear anatomy and suitability for implantation.
- Speech perception testing: Evaluates ability to understand speech with and without hearing aids.
- Psychological evaluation: Assesses motivation, expectations, and overall emotional well-being.
Surgical Procedure for Cochlear Implantation
Cochlear implant surgery is a delicate and typically outpatient procedure performed under general anesthesia. Here’s a breakdown of the process:
Preoperative Preparation:
- Detailed discussions: Extensive conversations with the surgeon and healthcare team to address all questions and concerns.
- Medical evaluations: Pre-operative tests and exams to ensure overall health and suitability for surgery.
- Medication adjustments: Stopping certain medications that could interfere with anesthesia or healing.
- Dietary restrictions: Specific instructions on fasting before surgery.
- Hair removal: May be necessary behind the ear for the incision site.
Types of Cochlear Implant Systems:
- Nucleus® cochlear implant system (Cochlear Americas): Most widely used globally, with various electrode configurations.
- MED-EL cochlear implant system (MED-EL USA): Known for innovative features like fine-tuning electrodes.
- Advanced Bionics cochlear implant system (AB): Offers hybrid implants for mixed hearing loss.
Surgical Techniques and Implant Placement:
- Incision: A small incision is made behind the ear, and the skin and underlying tissue are carefully lifted.
- Mastoidectomy: A portion of the mastoid bone (behind the ear) is drilled to access the inner ear.
- Cochleostomy: A small opening is created in the cochlea to insert the electrode array.
- Electrode placement: The surgeon carefully inserts the chosen electrode array into the cochlea, ensuring optimal placement and stimulation.
- Receiver/Stimulator placement: The internal receiver/stimulator is placed under the skin behind the ear.
- Closure: The incision is carefully stitched or closed with dissolvable sutures.
Additional notes:
- Surgery usually takes 2-3 hours.
- Most patients go home the same day or stay overnight for observation.
- Recovery generally involves pain management, wound care, and initial healing for several weeks.
- Activation and programming of the implant occur weeks later, followed by ongoing rehabilitation and adjustments.
Post-Implantation Rehabilitation and Programming
Getting a cochlear implant is just the first step. To maximize its benefits, thorough rehabilitation and programming are crucial. Here’s a breakdown of the crucial post-implantation processes:
Activation and Initial Programming:
- Activation: Weeks after surgery, the implant is switched on, and sound stimulation begins.
- Initial programming: An audiologist adjusts the implant settings to match your specific hearing needs and preferences. This involves fine-tuning parameters like stimulation levels, frequency maps, and sound processing strategies.
Auditory Training and Rehabilitation:
- Rehabilitation starts from day one: Exercises help the brain adapt to and interpret the new auditory information received through the implant.
- Speech therapy: Crucial for improving speech understanding and communication skills, especially for children.
- Auditory training: Exercises focus on sound discrimination, localization, and comprehension in various environments.
- Music therapy: Can enhance auditory skills and enjoyment of music.
- Family and community support: Encouragement and participation in communication activities are vital for success.
Follow-up Care and Adjustment:
- Regular appointments: Monitor progress, adjust programming, and address any concerns.
- Remote programming: Some systems allow adjustments via teleconference for convenience.
- Lifelong adjustments: Hearing needs and preferences may change over time, requiring ongoing fine-tuning.
Additional notes:
- Rehabilitation is an ongoing process, typically lasting months or even years.
- The pace and intensity of therapy vary depending on individual needs and progress.
- Patience, motivation, and active participation are essential for optimal outcomes.
- Support groups and online communities can offer valuable resources and connections.
Benefits and Limitations of Cochlear Implants
While cochlear implants are a remarkable technology offering incredible potential for restoring hearing, it’s essential to understand both their benefits and limitations to make informed decisions.
Benefits:
- Improved Speech Perception and Communication: This is the most significant benefit, allowing individuals with severe hearing loss to understand speech more clearly, especially in noisy environments. This drastically improves communication and social interaction.
- Enhanced Quality of Life: Studies show significant improvements in quality of life after cochlear implants, including increased social participation, employment opportunities, emotional well-being, and overall satisfaction.
- Greater Independence: Improved hearing can lead to increased independence in daily activities and reduce reliance on others for communication.
- Access to Sound Environment: Recipients can perceive a wider range of sounds, enriching their experience of the world around them.
- Potential for Music Appreciation: With advanced programming and training, some individuals can even enjoy and appreciate music to a certain extent.
Limitations:
- Not a Cure: Implants do not restore normal hearing. Sounds may still be perceived differently compared to natural hearing.
- Requires Rehabilitation and Adjustment: Extensive speech therapy, auditory training, and ongoing adjustments are crucial for success.
- Not Suitable for Everyone: Candidacy depends on specific hearing loss type, age, and individual needs.
- Financial Cost: Cochlear implants and their maintenance can be expensive, with varying insurance coverage depending on location.
- Surgical Risks and Complications: Like any surgery, there are potential risks and complications, although minimal and rare with modern techniques.
- Technical Limitations: While constantly improving, technology still has limitations in sound quality and naturalness.
- Lifelong Commitment: Maintenance, adjustments, and potential upgrades may be needed throughout life.
Challenges and Considerations:
- Realistic Expectations: It’s essential to have realistic expectations and understand that full restoration of natural hearing is not possible.
- Motivation and Commitment: Success requires a strong commitment to rehabilitation and ongoing adaptation.
- Support System: Having a supportive family and community network can significantly improve the adjustment process.
- Long-Term Maintenance: Costs and potential future upgrades should be considered.
- Individual Differences: Outcomes and experiences vary greatly between individuals depending on various factors.
Ultimately, the decision to pursue a cochlear implant is a personal one that requires careful consideration of the benefits, limitations, and individual circumstances. Consulting with specialists and understanding the specific details are crucial for making an informed and empowered choice.
Advances in Cochlear Implant Technology: Beyond the Basics
Cochlear implant technology continues to evolve, offering even more promising possibilities for individuals with severe hearing loss. Let’s explore some exciting advancements:
Wireless Connectivity and Accessories:
- Bluetooth compatibility: Some implants connect directly to smartphones, streaming audio for calls, music, and media directly to the implant, bypassing external processors.
- Remote adjustments: Telehealth appointments allow specialists to adjust and personalize settings remotely, enhancing convenience and accessibility.
- Assistive listening devices: Implants can connect seamlessly with microphones and other assistive devices, improving hearing in challenging environments.
Electrode Array Innovations:
- Multichannel electrodes: Arrays with dozens of individual electrodes stimulate specific regions of the cochlea, providing finer-grained sound information for improved pitch discrimination and clarity.
- Conformable electrodes: Flexible electrode designs minimize tissue damage and improve contact with the auditory nerve, potentially enhancing sound quality and reducing distortion.
- Drug-delivering electrodes: Research explores electrodes that release drugs to stimulate nerve growth or protect against degeneration, potentially improving long-term outcomes.
Future Directions in Research and Development:
- Artificial intelligence: Machine learning algorithms could personalize sound processing in real-time, adapting to individual preferences and environmental changes.
- Brain-computer interfaces: Direct neural stimulation bypassing the auditory nerve may offer new possibilities for hearing restoration.
- Regenerative medicine: Stem cell research aimed at regenerating damaged hair cells in the inner ear could potentially lead to natural hearing restoration in the future.
These advancements reflect the continuous effort to refine and improve cochlear implant technology. While some innovations are already available, others are still in research and development stages. Regardless, they point towards a future with even more effective and personalized hearing solutions for individuals with severe hearing loss.
Ethical and Social Implications
Cochlear implants, while offering tremendous benefits for individuals with severe hearing loss, raise important ethical and social considerations that deserve exploration.
Accessibility and Affordability:
- Cost: Cochlear implants and their maintenance can be incredibly expensive, limiting access for many, especially in countries with limited healthcare coverage. This raises concerns about equitable access and potential discrimination based on socio-economic status.
- Availability of specialists and rehabilitation services: Skilled surgeons, audiologists, and speech therapists are crucial for successful outcomes. Their limited availability in certain regions can further restrict access to cochlear implants.
Ethical Considerations in Implantation:
- Informed consent: Ensuring thorough and understandable information is provided to both individuals and their families before deciding on implantation, especially when children are involved.
- Autonomy and self-determination: Respecting individual choices and cultural perspectives on deafness and hearing restoration. Consider the Deaf community’s concerns about cochlear implants as a potential erasure of their cultural identity and language.
- Long-term effects and unforeseen risks: Openly discussing the potential long-term effects and any unknown risks associated with cochlear implants.
Societal Perspecnd Collaboration:
These complex ethical and social issues require ongoing dialogue and collaboration among various stakeholders, including healthcare professionals, researchers, deaf communities, policymakers, and individuals considering cochlear implants. It’s crucial to ensure accessibility, respect diverse perspectives, and promote understanding and inclusion for all involved.
Success Stories and Testimonials: Hearing the World Anew with Cochlear Implants
The lives of countless individuals, young and old, have been transformed by the gift of sound thanks to cochlear implants. Hearing personal stories and testimonials offers a powerful glimpse into the real-life impact of this technology on individuals and families:
1. Regaining Independence and Connection:
- John, 58: Diagnosed with profound hearing loss in his late 40s, John struggled to engage in conversations, participate in social activities, and even follow conversations at home. After receiving cochlear implants, John describes regaining “a piece of my life” – confidently navigating work meetings, enjoying phone calls with friends, and reconnecting with his family on a deeper level.
2. Unlocking the World of Music:
- Sarah, 12: Born with severe hearing loss, Sarah had limited access to music throughout her childhood. With cochlear implants, she describes experiencing music for the first time as “magical.” Now, she actively participates in her school choir, learning to play instruments, and discovering the joy of music in her daily life.
3. Overcoming Challenges and Inspiring Others:
- Maria, 35: A single mother with progressive hearing loss, Maria faced communication barriers at work and struggled to connect with her young daughter. After implantation, she regained confidence at work, leading presentations and collaborating effectively. She shares her story publicly, inspiring others with hearing loss to pursue cochlear implants as a path to a fulfilling life.
4. Breaking Down Communication Barriers:
- David, 72: Diagnosed with age-related hearing loss, David felt increasingly isolated, withdrawing from social gatherings and struggling to follow conversations. Cochlear implants have helped him reconnect with his loved ones, participate actively in community events, and rediscover the joy of meaningful conversations.
5. Embracing a New Future:
- Emily, 2: Diagnosed with profound hearing loss at birth, Emily’s early development was impacted by limited auditory input. Receiving cochlear implants at a young age opened a world of sound and language acquisition. Today, Emily thrives in school, engages actively with her peers, and enjoys the wonders of her auditory world.
These stories represent just a small sample of the countless individuals whose lives have been enriched by cochlear implants. Each journey is unique, filled with challenges and triumphs, but ultimately celebrating the power of hearing and its impact on individual potential and social connection.
Conclusion and Future Outlook
Our exploration of cochlear implants has revealed a fascinating world of technology, potential, and ethical considerations. These remarkable devices offer individuals with severe hearing loss a chance to reconnect with sound, improve communication, and lead fuller lives. While challenges remain in accessibility and ethical considerations, ongoing research and innovation promise a future with even more refined and personalized solutions. By fostering collaboration and prioritizing inclusivity, we can create a brighter hearing future where everyone can access the wonders of sound. Remember, the decision to pursue cochlear implants is personal, and I encourage you to continue exploring this field and consider its possibilities in your own unique context.
FAQs about Cochlear Implants:
1. How much do cochlear implants cost?
Cochlear implants are expensive, typically ranging from $30,000 to $50,000 per ear without insurance. Thankfully, most major insurance companies and federal programs like Medicare and Medicaid cover some or all of the cost.
2. Am I a candidate for cochlear implants?
Several factors determine candidacy, including the type and severity of your hearing loss, age, overall health, motivation, and realistic expectations. Consulting with an audiologist and ENT specialist is crucial for an accurate assessment.
3. What is the surgery like?
Cochlear implant surgery is typically an outpatient procedure performed under general anesthesia. It involves making an incision behind the ear, creating an opening in the cochlea, and carefully inserting the electrode array. Recovery usually takes several weeks.
4. Do cochlear implants restore perfect hearing?
While cochlear implants significantly improve hearing, they don’t restore it to “normal.” Sounds may still be perceived differently, and speech understanding requires ongoing rehabilitation and training.
5. What are the benefits of cochlear implants?
The main benefits include improved speech understanding and communication, increased quality of life, greater independence, and access to the broader sound environment. Some individuals even experience the joy of music appreciation.
6. What are the risks and limitations of cochlear implants?
Like any surgery, there are potential risks like infection or device malfunction. Additionally, not everyone qualifies, and costs can be a barrier. Realistic expectations and understanding the limitations are crucial before considering implantation.
7. What are the latest advancements in cochlear implant technology?
Exciting advancements include wireless connectivity, finer electrode designs, and potential future directions like AI and brain-computer interfaces aimed at improving sound quality, personalization, and accessibility.
8. Are cochlear implants ethical?
Ethical considerations like accessibility, informed consent, and respect for diverse perspectives on deafness require ongoing dialogue and collaboration among stakeholders.
9. Where can I find success stories or testimonials about cochlear implants?
Many organizations and online communities share inspiring stories of individuals whose lives have been transformed by cochlear implants. These personal experiences offer valuable insights into the real-world impact of this technology.
10. What does the future hold for cochlear implants?
The future is bright, with ongoing research and innovation promising more affordable, accessible, and personalized solutions. Advancements in miniaturization, biocompatibility, and sound processing offer the potential for even greater hearing restoration for individuals with severe hearing loss.
Read More:
Affordable Hearing Aids for Seniors: Enhancing Wellness with Budget-Friendly Solutions
Hearing Aid Waivers in the US Army: Can You Serve with Hearing Loss?
Resound vs Unitron Hearing Aids: Unlocking the Ultimate Hearing Experience
Hearing Aid Replacement: Empowering Solutions for Improved Hearing Health
A Guide to iPhone Hearing Aids: Unlocking Clearer Connections